The Pediatric Liver Transplant Program is a collaborative initiative between the Section of Transplant Surgery and the Division of Gastroenterology, Hepatology & Nutrition, jointly operated by St. Louis Children’s Hospital and WashU Medicine’s Department of Pediatrics. Together, these teams provide comprehensive, world-class care for children with liver disease.
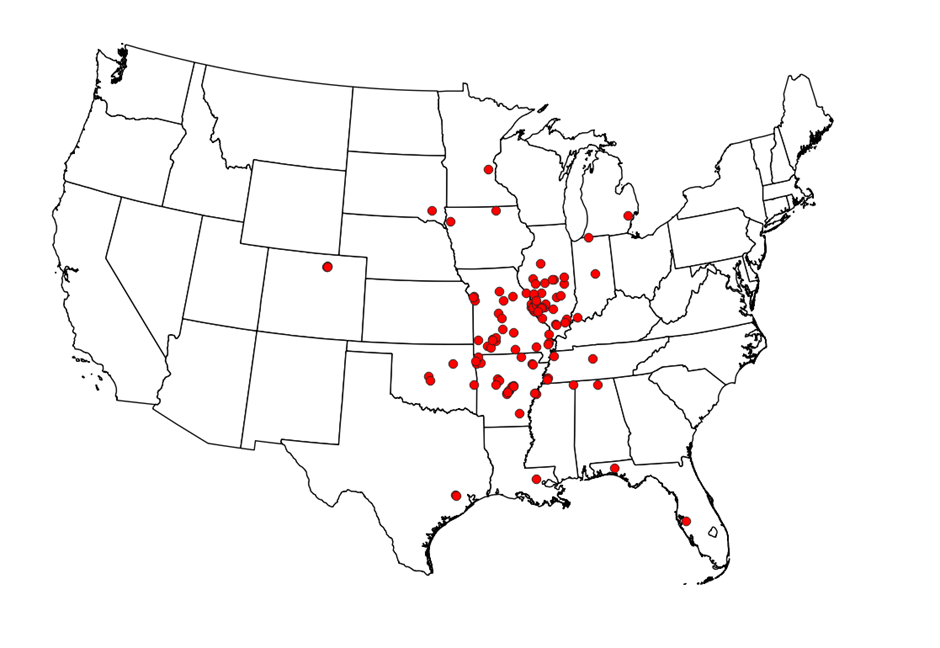
The Pediatric Liver Program is a full-spectrum subspecialty service with recognized expertise in diagnosing and managing all forms of pediatric liver disease. It partners with the Central Midwest Transplant Service, a leading regional, national, and international referral center with extensive experience in liver, kidney, and small intestine transplantation.
Guidelines for referral & access
Contacts for referral & advice
Mission
To deliver thorough evaluation, treatment and care for children with liver disease—including those with end-stage or life-threatening conditions requiring liver transplantation or major surgical procedures such as liver resection.
To optimize outcomes and expand donor options by offering all current forms of liver transplant surgery, including:
- Living-related segmental transplants
- Cadaveric segmental transplants
- Split-liver transplants
- Whole liver transplants
Clinical activities
History & innovation
Since 1985, pediatric liver transplants have been performed at St. Louis Children’s Hospital/WashU Medicine. Over 80 infants, children and adolescents with end-stage liver disease have successfully undergone transplantation—including infants as small as 3 kg (9 lbs).
The program has pioneered advanced surgical techniques to expand donor eligibility and improve outcomes:
- Segmental liver transplants
- Living-related transplants
- Split-liver transplants, enabling adult donor organs to be adapted for use in very small infants
Today, the program achieves world-standard survival rates of 95% at 1, 3 and 5 years, with excellent long-term quality of life for most patients.
Patient care approach
Early consideration of liver transplantation is critical once end-stage liver disease is diagnosed. At SLCH, potential transplant candidates undergo a comprehensive evaluation over 1–3 days, which includes:
- Diagnostic review and treatment history
- Imaging studies and coordinated lab testing
- Specialist consultations across disciplines
Following this evaluation, the transplant team meets with families for a detailed discussion of:
- Diagnosis and treatment options
- Prognosis and potential outcomes
- Recommended care plans
A personalized pre- and peri-transplant plan is developed, with close collaboration among surgeons, physicians, nurse practitioners and transplant coordinators. Post-transplant care is equally robust, supported by:
- Experienced transplant intensive care specialists
- Family education and psychosocial support resources
- Seamless coordination across SLCH and WashU Medicine services